It was awful. Fever approaching 104, body aches everywhere, an unremitting headache. It seemed that last week I, like 9.7 million other Americans in the months before me, had caught the flu.
Luckily, as a clinician, I had already taken the flu shot months earlier. And luckily, as a clinician, I knew that when my primary care doctor took a rapid-analysis flu swab in her office that came back negative, I nevertheless most likely had the flu. Accordingly, I still took the antiviral medication Tamiflu because I knew it could help diminish the length or the severity of my symptoms, and crucially, I was very cautious to avoid exposure to those near me by using a face mask and practicing good hand hygiene.
Accurate and prompt diagnosis of flu is key for patients to improve their likelihood of survival.
We already face many challenges in fighting a common but potentially deadly disease, one that is particularly potent this year. One of the most insidious is that many people are often carriers of flu without even knowing it (even if they feel it).
Just because you’ve gotten a flu shot doesn’t mean you can’t get the flu, so that possibility shouldn’t be dismissed when you come down with flu-like symptoms. Moreover, the rapid tests utilized in doctors’ offices nationwide to confirm its presence often give misleading results — as they did in my case — reassuring someone that they aren’t infected when the reverse is true. These phenomena put us at risk for an epidemic of underdiagnosed flu — people not receiving potentially helpful treatment and not taking proper precautions to avoid its spread because they don’t know any better.
This complicated problem of underdiagnosed flu is seen in the inpatient setting, as well. One recent analysis noted that nearly half of patients admitted with shortness of breath and fever that were ultimately found to have flu were not initially tested for it on presentation to the hospital.
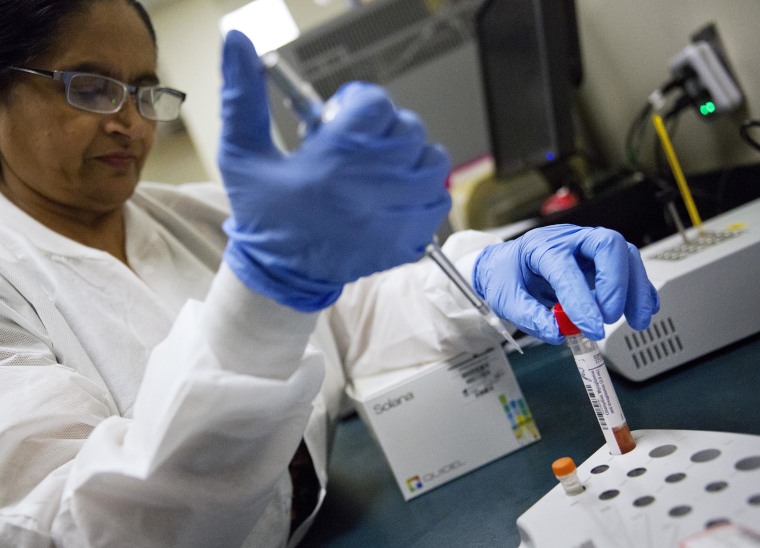
The rapid influenza diagnostic test given in doctors’ offices, which detects the presence of proteins found on the surface of flu viruses, is increasingly common nationwide as it becomes available in most clinical settings. But it is commonly falsely negative, particularly when overall rates of flu are high in the surrounding community.
These delays in diagnosis or underdiagnosis can clearly put the public at greater risk of flu outbreaks. Flu is easily transmissible by air droplet: A simple cough from an infected source will expose an entire cabin filled with passengers in a jetliner within minutes.
Second, accurate and prompt diagnosis of flu is key for patients to improve their likelihood of survival. While commonly prescribed medications like Tamiflu cannot completely treat flu like an antibiotic can treat a bacterial illness, it does reduce the length and severity of symptoms if started within 48 hours of symptom onset.
Further, with a host of new and potentially dangerous mimickers of flu on the horizon, such as the new SARS-like virus seen in China this month, it is important to understand quickly whether influenza is present or not so that attention and treatments can shift accordingly.
We should be moving away from the broad use of this test, as major organizations such as the Infectious Diseases Society of America have recommended, given that false negative rates can approach 30 percent (!). That’s unacceptably high and makes a negative result virtually worthless as a guide for what to do.
Instead, we should be encouraging the adoption and affordability of innovations that are starting to address the limitations of the existing rapid test, including a relatively new rapid molecular assay associated with lower false-negative rates. Right now, this test is not as widely available nationwide as the original rapid flu test in outpatient clinics, likely because of the added cost to utilize it at scale, thus limiting its impact.
And while getting a flu shot doesn’t fully innoculate you from the illness, it is still tremendously beneficial. The evidence is clear that the vaccine diminishes risk of infection by at least half depending on the season (this year, it’s near that threshold per the CDC). Moreover, in cases when infection still occurs, it reduces the severity of the illness considerably. Regrettably, skepticism about flu vaccine efficacy remains disappointingly widespread, even though none of the counterarguments on vaccination are remotely rooted in science.
While getting a flu shot doesn’t fully innoculate you from the illness, it is still tremendously beneficial.
Influenza has reached almost mythic status as a potential cause of human extinction for a good reason: The last time a large swath of humanity died in short order, it was the result of the 1918 Spanish Flu Pandemic. One-third of the world’s population (500 million at the time) became infected, and nearly 50 million people died globally; that’s 10 million more than were killed in the Great War that preceded it.
We don’t need to panic. But we do need our health care professionals and elected leaders to ensure that our nation’s providers and clinics have the right tests and resources to safeguard public health. Meeting this need should be a requirement of effective leadership, especially given the gravity of a potential flu outbreak for Americans of all ages.